Treatment of Sleep Apnea
If you’ve been treated for sleep apnea, you’ve probably tried a CPAP machine. And while CPAP is highly effective, many patients struggle to use it. We offer a comfortable solution that’s ideal for patients who have difficulty using CPAP: Oral Appliance Therapy.
Oral Appliance Therapy
- Custom fit to your mouth
- Eliminates snoring
- No replacement parts needed
- Not disruptive for your bed partner
- Scientific studies validate the effectiveness of oral devices for most cases of sleep apnea.
- Effective because it is often preferred by patients
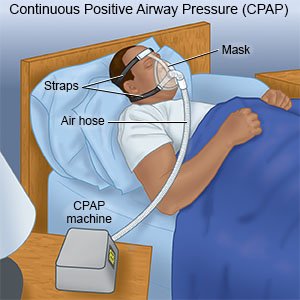
CPAP
- Hoses connect machine to your face
- Periodic hose replacements are necessary
- Air filter/humidity filter requires maintenance and replacement
- Not recommended for patients with claustrophobia
- Skin irritation may be created by the face mask
- Sleeping body position is limited due to importance of mask seal.
- Must be examined by airport security
- Sound / look of machine may have an impact on bed partner
If you are considering using an oral appliance, here are the most frequently asked questions about Oral Appliance Therapy
What is an Oral Appliance Therapy?
It is a removable device worn in the mouth during sleep that helps control sleep apnea and snoring, thus improving sleep quality. The appliance gently positions the lower jaw and tongue slightly forward. This opens space in the back of the throat and reduces tissue obstruction to help keep your airway open and clear during sleep.
What are the benefits of Oral Appliance Therapy?
Sleep Apnea may pose serious health risks since it disrupts normal sleep patterns and can reduce normal blood oxygen levels. This can result in problems such as daytime sleepiness, driving and work related accidents, irregular heartbeats, high blood pressure, heart disease, stroke, obesity, and memory and learning problems. By wearing an oral appliance during sleep, your body may be able to maintain higher blood oxygen levels and lessen the severity of problems associated with sleep-disordered breathing.
What are the risks of wearing an Oral Appliance during sleep?
Short-term side effects may include excessive salivation, difficulty swallowing with the appliance in place, sore jaws, sore teeth, jaw joint pain, dry mouth and short term bite changes. Most of these side effects are minor and resolve quickly on their own. Long-term complications may include permanent and significant bite changes as a result of wearing an Oral Sleep Appliance. Follow- up visits with the provider of your oral appliance are needed to ensure proper fit and effectiveness.
What are the alternatives to Oral Appliance Therapy?
Other accepted treatments for sleep-disordered breathing may include behavioral modifications, continuous positive airway pressure (CPAP) and various surgeries.
What are the post-treatment considerations?
Follow-up visits with your provider are mandatory to ensure a proper fit and to examine your mouth to ensure a healthy condition. Alert your provider if you experience any changes. After fitting your Sleep Appliance, a sleep study is necessary to objectively ensure effective treatment.
Diagnosis
Your health care provider may make an evaluation based on your symptoms and a sleep history, which you can provide with help from someone who shares your bed or your household, if possible.
You’re likely to be referred to a sleep disorder center. There, a sleep specialist can help you determine your need for further evaluation.
An evaluation often involves overnight monitoring of your breathing and other body functions during sleep testing at a sleep center. Home sleep testing also might be an option. Tests to detect sleep apnea include:
- Nocturnal polysomnography. During this test, you’re hooked up to equipment that monitors your heart, lung and brain activity, breathing patterns, arm and leg movements, and blood oxygen levels while you sleep.
- Home sleep tests. Your health care provider might provide you with simplified tests to be used at home to diagnose sleep apnea. These tests usually measure your heart rate, blood oxygen level, airflow and breathing patterns. Your provider is more likely to recommend polysomnography in a sleep testing facility, rather than a home sleep test, if central sleep apnea is suspected.
- If the results aren’t typical, your provider might be able to prescribe a therapy without further testing. Portable monitoring devices sometimes miss sleep apnea. So your health care provider might still recommend polysomnography even if your first results are within the standard range.
If you have obstructive sleep apnea, your health care provider might refer you to an ear, nose and throat specialist to rule out a blockage in your nose or throat. An evaluation by a heart specialist, known as a cardiologist, or a doctor who specializes in the nervous system, called a neurologist, might be necessary to look for causes of central sleep apnea.